Facts About PCOS and Pregnancy
Polycystic ovary syndrome (PCOS) is one of infertility's most common but treatable causes. Here’s what you need to know to increase your chances of conceiving.
Approximately 5 million people in the United States are affected by polycystic ovary syndrome (PCOS), making it one of the most common metabolic and hormonal disorders for people ages 18 to 44. Despite being prevalent, diagnosis can be difficult because certain symptoms (fatigue, irregular or heavy periods, acne, weight gain) have a variety of potential causes. Unfortunately, people often experience symptoms for years—including infertility—before receiving a proper diagnosis.
If you suspect you’re struggling with PCOS, identifying the key signs and talking to your doctor is the best place to start. Voicing your concerns will help you to receive the treatment needed to improve your odds of conceiving. Even if you’re not trying to get pregnant, early diagnosis and treatment for PCOS are essential for lowering the risk of long-term complications, such as type 2 diabetes and heart disease.
What Causes PCOS?
The exact cause of PCOS is unknown, but there’s evidence that the condition is genetic, meaning you might be more likely to develop PCOS if a family member has also dealt with it at some point. Additionally, environmental factors are believed to play a role in PCOS, though research on this correlation is ongoing.
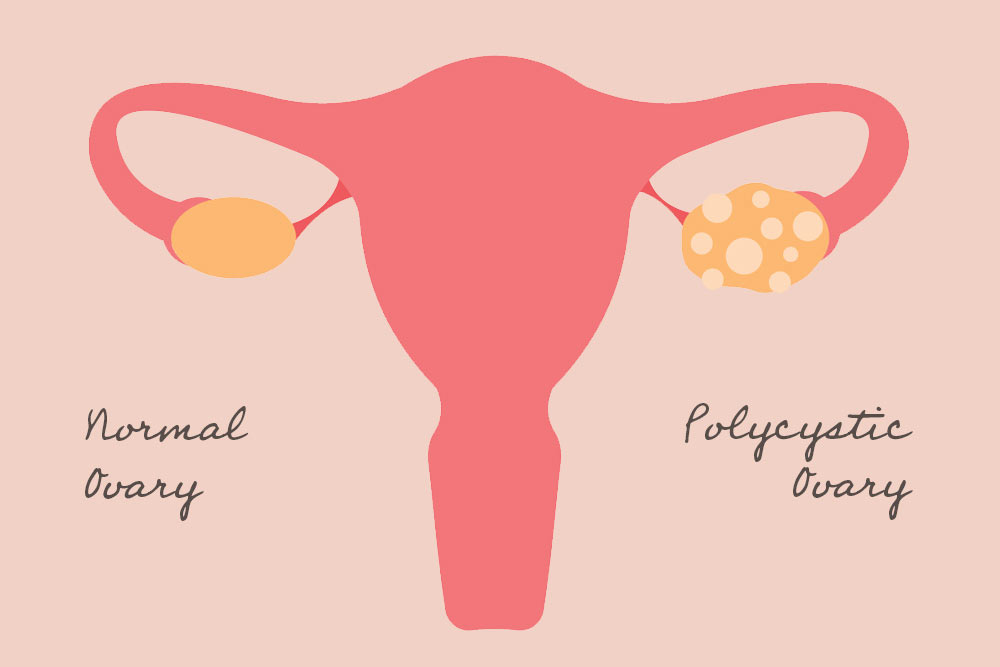
Scientists do know that this syndrome causes a person’s ovaries (the organs that produce and release eggs) to create an excess of the male sex hormone called androgens, leading to reproductive hormones becoming imbalanced in women and people assigned female at birth (AFAB). As a result, this can lead to irregular or missed periods, unpredictable ovulation, and tiny fluid-filled sacs (also referred to as follicles or cysts) that develop on the ovaries. These cysts are not dangerous or painful (unlike endometriosis), and it’s possible to have polycystic ovary syndrome without ovarian cysts.
What Are the Signs and Symptoms of PCOS?
Polycystic ovarian syndrome has many symptoms, and it’s common for women and people AFAB only to exhibit a few, or many, at a time. According to John Hopkins Medicine, the typical signs of PCOS include:
- Infertility
- Missed periods, irregular periods, or very light periods
- Larger ovaries or ovaries containing many cysts
- Excess hair growth on the chest, stomach, and back
- Weight gain, especially in the abdominal area
- Oily skin and acne
- Baldness or thinning hair
- Skin tags on the neck or armpits
- Dark or thick skin patches on the back of the neck, in the armpit area, or underneath the breasts
PCOS is diagnosed by your doctor. In addition to asking questions about your medical history and current symptoms, your health care provider will also perform a physical exam and may recommend an ultrasound or a blood test for further diagnosis.
How Does PCOS Affect Pregnancy?
PCOS can make it difficult to get pregnant naturally because ovarian cysts interfere with ovulation. Between 70-80% of people with polycystic ovary syndrome are infertile; however, you can increase your chances of conception with a specialist’s guidance and fertility treatments.
People with PCOS are also three times as likely to experience early pregnancy loss. According to a 2023 study by the Journal of Clinical Endocrinology and Metabolism, the medication metformin (typically used to treat type 2 diabetes) may help to reduce the chance of miscarriage in these types of cases.
In addition, PCOS is related to an increased risk of the following pregnancy complications:
Gestational Diabetes
This type of diabetes only affects pregnant people and, when treated properly, will generally resolve after delivery. Babies whose birth parents have gestational diabetes can be larger for their gestational age, have lower blood sugar levels, and have trouble breathing following birth. For the birth parent, the risk of cesarean delivery is increased due to the baby’s size. Additionally, birth parents with gestational diabetes and their babies are at a higher risk for type 2 diabetes later in life.
Preeclampsia
Characterized by high blood pressure that spikes in the second half of pregnancy (after the 20-week mark), preeclampsia can cause damage to organ systems in the birth parent’s body, most often the liver and kidneys, and in some cases, the brain. When left untreated, preeclampsia can turn into eclampsia, a rare, life-threatening condition that can lead to seizures and even death.
Preterm Birth
Newborns are considered preterm if delivered before 37 weeks of pregnancy. These preemies can suffer lifelong effects, such as poor health and growth, visual and hearing impairments, learning disabilities, and more.
What Should I Do if I’m Trying To Conceive?
If you’re interested in getting pregnant in the future, talk with your doctor about planning for a healthy pregnancy and delivery.
Starting at a healthy weight before conception is especially important because obesity can increase the risks of severe pregnancy complications for people with PCOS. Lifestyle choices such as diet and exercise can help with arriving at and maintaining a healthy weight and lowering inflammation, which is shown to affect those suffering from PCOS as well.
Balancing your blood sugar levels is also recommended when experiencing problems with fertility because PCOS can change how your body uses insulin. This vital hormone transports glucose (sugar) in the body for optimal production. In addition to diet, exercise, and some cases, medication, your blood sugar levels can improve.
Additionally, tracking your ovulation and using at-home tests can help you monitor your cycle and identify your ovulation window, the six to seven days a month you can get pregnant, and the best time to try and conceive.
If you decide to work with a fertility specialist, they may recommend medications, such as Clomid, metformin, or birth control, for balancing your hormones. Sometimes, your provider may advise reproductive technology (IVF) to help you get pregnant.
Does PCOS Affect Breastfeeding?
According to La Leche League International, people with PCOS may struggle to produce enough breast milk or may make an overabundance of it. Once again, early intervention during pregnancy is essential for helping to balance hormones and decrease hormonal disruption before baby arrives. Parents can also seek lactation support during pregnancy to establish strategies should problems occur.
The PCOS Awareness Association (PCOSAA) encourages birth parents to breastfeed their babies and says it is safe to nurse even if you’re on insulin medication, such as metformin or glyburide. Breastfeeding lowers a baby’s risk of childhood obesity and type 2 diabetes later on in life; for birth parents with gestational diabetes, nursing lowers the increased risk of developing type 2 diabetes as well as possibly helping them return to a healthy weight after birth.
For those with polycystic ovary syndrome, it’s important to continue managing symptoms post-delivery, even if symptoms appear less severe. PCOSAA explains that hormonal fluctuations after pregnancy and during breastfeeding can change the symptoms a person experiences, and it may take some time for a birth parent to settle into their new “normal.”
Though PCOS is common, it’s still difficult to endure in everyday life and incredibly challenging if trying to conceive. Your doctor is the best resource for receiving help and support and navigating decisions along the way. Don’t hesitate to reach out sooner than later if you feel you are affected by PCOS, and know that management—and symptom improvement—is available.








