Monkeypox and Pregnancy: What You Need to Know
The risks, symptoms, treatment options, and how the virus may affect labor and delivery.
Medical Expert: Brenna L. Hughes, MD, MSc
The monkeypox virus reemerged in the U.S. in March of this year and cases have continued to grow in number, totaling over 24,000 to date. While that figure may appear relatively small, the White House declared monkeypox a public health emergency in August, following the World Health Organization (WHO) calling the global outbreak an international concern in July.
In a world still reeling from the coronavirus pandemic, such announcements create chaos and confusion, especially for higher-risk populations like pregnant people.
If you’re expecting, you likely have questions and concerns about the monkeypox virus outbreak and how it can affect your pregnancy. Brenna L. Hughes, MD, MSc, a maternal-fetal medicine specialist with Duke Health in Durham, North Carolina answers some of these pressing questions and shares what you need to know while pregnant.
What Is Monkeypox?
The Centers for Disease Control and Prevention (CDC) says that monkeypox is a rare disease caused by infection with the monkeypox virus. Monkeypox virus is grouped alongside the variola virus, the virus that causes smallpox. These two viruses share symptoms, but thankfully, monkeypox symptoms are milder and infection rarely results in death.
There are different types of monkeypox virus: Clade I and Clade II, the latter of which includes infections from the current outbreak. The good news is that over 99% of people who contract Clade II are expected to survive. However, the CDC states that people with weakened immune systems, children under age 8, people with a history of eczema, and people who are pregnant or breastfeeding may be more likely to experience an infection that results in serious illness or death.
Monkeypox is a direct contact infection, meaning the virus can spread through close contact with an infected person or animal via rashes, scabs, or bodily fluids, including saliva. You can also become infected through animal bites or scratches, or by consuming uncooked meat of an infected animal, specifically wild game, such as squirrels. Additionally, home textiles, such as bedding and blankets, can also transmit monkeypox if handled by someone infected with the virus.
Are There Risks to Pregnant People?
Research on the associated risks and effects of monkeypox in pregnancy is still ongoing, therefore, clarity—and peace of mind—is limited.
“The answer to this question [of risk to pregnant people] is not completely known because there are very few reports of monkeypox in pregnancy and they are not from the current outbreak,” explains Dr. Hughes. “Based on those few reports there is concern that pregnancy could be a risk factor for severe disease.”
She also adds there is a concern that the virus can be passed to the fetus, causing infection or death in the unborn baby.
“This has been seen with some other pox viruses, but we don’t know at this point whether it will happen with the current circulation strain of monkeypox in the U.S.”
While this information is certainly concerning, it’s important to understand that maternal and neonatal outcomes are not fully known because there are few reports to draw from. Still, it’s crucial to be informed and take precautions during pregnancy to best safeguard against illness and protect your and your baby’s health.
What Are the Signs and Symptoms of Infection?
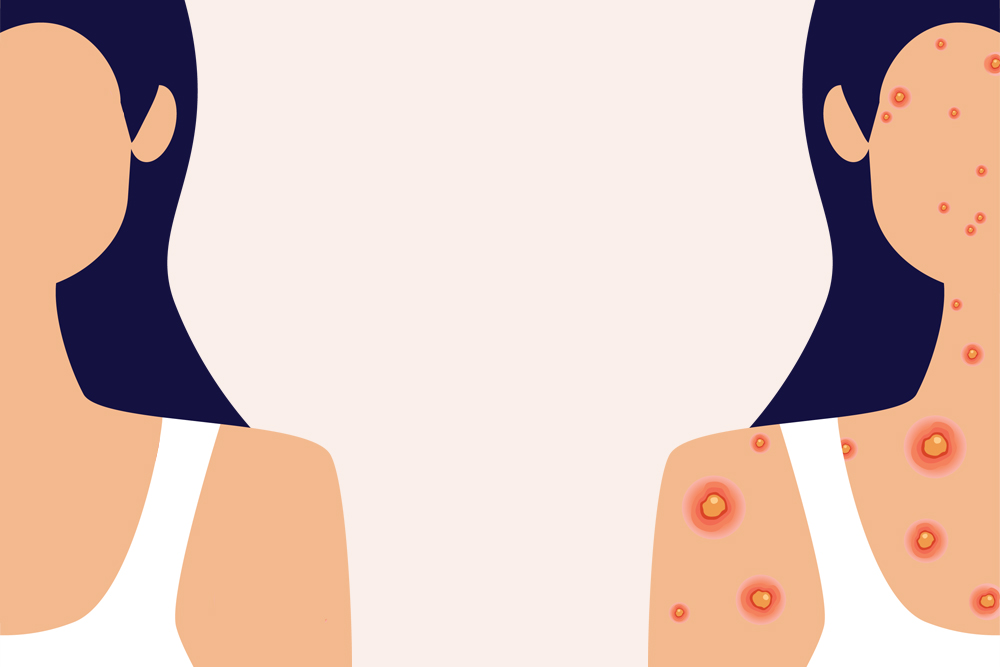
Monkeypox is commonly associated with a rash that can appear like pimples or blisters on the face, inside the mouth, and on other parts of the body, including the hands, feet, chest, and genitals. These often painful, itchy pimples and blisters fill up with pus, scab over, and eventually fall off over a period of two to four weeks.
Additional symptoms include fever, headache, muscle aches, chills, tiredness, and swollen lymph nodes. According to the Mayo Clinic, monkeypox symptoms may start five to 21 days after exposure; the telltale rash specifically appears one to four days after the onset of a fever.
For pregnant people, Dr. Hughes says the typical symptoms are similar to nonpregnant people (perhaps even more so when it comes to fatigue and general lethargy), though those expecting should be wary of possible dehydration from a fever.
“For pregnant people, if they were to experience fever or dehydration they may also experience contractions. So keeping well-hydrated is important.”
If you experience any of the symptoms listed above or show signs of a developing rash or other skin condition, contact your health care provider immediately, even if you do not know someone with the monkeypox virus.
How Does Infection Affect Labor and Delivery?
If a pregnant person is positive for infection upon arrival to their birthing facility, they will most likely be able to have a normal labor and delivery with a few additional precautions, says Dr. Hughes.
“[Medical staff] in their room will wear protective gear to prevent exposure as we do with any infection that can be spread to health care workers. If the patient has active genital lesions, a health care provider may consider a cesarean section.”
However, the American College of Obstetrics and Gynecologists (ACOG) states that the present data is “insufficient to demonstrate that cesarean section reduces the risk of perinatal infection or adverse outcomes.” More data is required to better understand the timing of transmission to the fetus in order to determine the safest method of delivery. As with all decisions regarding C-sections, it should continue to be an individualized discussion and choice between a pregnant person and their provider, taking into account the limited information available on monkeypox transmission during pregnancy and delivery.
Once a baby is born, both the CDC and the American Academy of Pediatrics (AAP) recommend separation from the infected birth parent until the virus clears, explains Dr. Hughes, as separation (including separate rooms) of a patient with monkeypox and their newborn is the best way to prevent transmission to the baby.
Additionally, the ACOG notes that while the benefits of skin-to-skin contact after childbirth are well-documented, direct contact between the birth parent and newborn is not advised until the skin lesions have resolved and a fresh layer of intact skin has formed. The same precautions are being taken with breastfeeding parents to avoid physical contact with the baby. It is unknown if the monkeypox virus is present in breast milk, so expressed breast milk from a patient who is isolated should be discarded until breastfeeding is reintroduced.
Breastfeeding parents should seek the guidance of a lactation consultant to offset potential complications from delayed breastfeeding.
What Can Pregnant People Do To Stay Safe?
The greatest risk factor, according to Dr. Hughes, is close contact or sexual contact with someone infected by the monkeypox virus. Therefore, the best way to prevent illness is to avoid close exposure to someone with active monkeypox infection.
Second to that, avoiding skin-to-skin contact with anyone who has a rash that looks like monkeypox, or with objects and materials that a person with monkeypox has used is recommended by the CDC.
As with all contagious diseases, washing your hands with soap and warm water and using alcohol-based hand sanitizers is a good idea, especially before eating or touching your face.
Of the two vaccines available for monkeypox, JYNNEOS and ACAM2000, Dr. Hughes says that JYNNEOS is considered the safe option for pregnant women, as studies of the vaccine in animals have shown no evidence of harm to a developing fetus. (There is insufficient human data surrounding vaccine-associated risks in pregnancy.) That being said, pregnant people should also be aware that this vaccine has not been evaluated in people who are breastfeeding or in young children and discuss their concerns with their physician.
In terms of treatment, there is no method specifically for monkeypox. However, Dr. Hughes says there is an antiviral medication that can be used in pregnancy if a patient’s care team recommends it.
For more information on the monkeypox virus and how to avoid transmission, visit cdc.gov.








