A Look at IVF in a Post-Roe World

With so much uncertainty, patients and physicians are burdened to carry the fear—and the threat—of the unknown.
Expert Sources: Lauren Berson, CEO and founder of Conceive; Eran Eshed, CEO and co-founder of Fairtility; David Sable, MD; Sophia Yen, MD, MPH, co-founder and CEO of Pandia Health
The overturning of Roe v. Wade in June 2022 sent a tidal wave of emotions and disbelief across the nation. For many, the feelings of panic, fear, and anger were palpable as the historical news sunk in that women’s health care as we have known it for nearly 50 years was forever changed.
To date, there are 13 states with abortion bans, 12 of which do not make exceptions for rape or incest, and an additional five states (Georgia, Arizona, Florida, Utah, and North Carolina) with gestational limits of 20 weeks or less. Georgia, for example, has a restriction on abortion after six weeks, which is often weeks before a person knows they are pregnant or can even be seen by an obstetrician to confirm a pregnancy.
Conception occurs around 14 days after a missed period, though it can be difficult to pinpoint exactly when sperm fertilized an egg. Therefore, “six weeks pregnant” can actually mean the embryo just started developing four weeks ago. This six-week restriction is just one of the many new laws affecting access to abortion care and impacting the lives of countless Americans.
For decades, discussions of who receives an abortion and why have been widely politicized and stigmatized, though the reality is that abortion access is a major part of reproductive care as a whole and impacts the community at large—including present and future in vitro fertilization (IVF) patients. Because IVF is assisted reproduction, it might be assumed that has no connection to abortion, yet it’s heavily impacted by decisions concerning reproductive rights.
IVF is a type of assisted reproductive technology (ART) that can aid with fertilization, embryo development, and implantation to increase your chances of getting pregnant. A combination of medications and surgical procedures are used to retrieve eggs from the ovaries to be fertilized by sperm in a lab. These fertilized eggs (embryos) are then implanted into the uterus in hopes of resulting in a conception and live birth.
So, what does IVF have to do with abortion? In short: It’s (almost) all about the embryo.
“The objective of IVF is to get you as many embryos as possible to build the family you’re looking to build. For example, someone might only want one child but has four frozen embryos,” says Lauren Berson, CEO and founder of Conceive. “Since the overturning of Roe. v. Wade, there has been discourse around whether the embryos created through IVF could be entitled to something called ‘personhood,’ which means if an embryo is considered a person at fertilization, it may limit what you’re able to do with that embryo.”
This grouping together of abortion services and options for embryos (including implantation, disposal, and donation, whether to research or to other intended parents) has created confusion for patients, physicians, and the general public, prompting the questions: What is considered a termination of life? And when does life begin?
Part of the issue with these newly enacted laws is that there is no clear, single definition of the word “abortion,” and this vague language can impact IVF. Additionally, many abortion bans are written with surgical abortion in mind (versus a medication abortion or a life-saving surgery for a pregnancy complication), further impeding the conversation around the need for reproductive care.
David Sable, MD, a retired reproductive endocrinologist in New York explains that this argument over embryos compromises the efficiency of the IVF process and is a step backward.
“One of the most important aspects of successful IVF—the ability to mature and develop a number of [embryos] in parallel during a single cycle—is at odds with a common element of many of the proposed post-Roe v. Wade repeal laws, the so-called ‘personhood’ provisions, which ‘give from the moment of sperm-egg fertilization, inalienable rights, equality of justice, and due process of law protection to embryos.’
“Much like the human reproductive system that it treats, one that creates many more mature eggs and embryos than will result in viable pregnancies, IVF matures and fertilizes many eggs per cycle. Like in nature, some will develop into viable pregnancies; most will not. Overcoming this inefficiency had to be engineered into the IVF procedure for it to have any chance of working at scale. Forty years of steady progress suggest that we made the right decision,” says Dr. Sable.
Eran Eshed, CEO and co-founder of Fairtility, a company that seeks to empower IVF through artificial intelligence, agrees that the implications of abortion bans could impact how IVF is performed, adding, “Currently, egg collection and fertilization include multiple egg fertilizations to determine which embryo would be the best choice for implantation to live birth. As of now, the success rate of IVF is 30% per cycle, with success rates dropping as patients age, so limiting egg retrieval and fertilization to one per cycle reduces the probability to ‘needle in a haystack’ odds. Of course, the repercussions would be devastating and financially crippling for prospective parents, as each cycle allowing for multiple egg retrieval can cost anywhere from $15,000 to $25,000. Requiring increased cycles [to only use one embryo at a time] would significantly reduce access to IVF treatment.”
And while efficiency and cost are inarguably important aspects of in vitro fertilization, the bigger picture here is upholding one’s right to their autonomy.
“Abortion care and fertility care are both connected to reproductive health and the ability to control one’s fertility,” says Eshed. “Fertility care can include a variety of services such as fertility testing, fertility treatments, and contraception, all of which are aimed to help individuals or couples become pregnant or avoid pregnancy. Access to both abortion and fertility care allow for informed decisions about reproductive health and family building.”
Unfortunately, the negative effects of post-Roe on IVF are not confined to just conversations surrounding embryos. There are many other potentially life-changing complications, circumstances, and outcomes to consider, all under the pressure of repeal laws written with vague language that make it hard to decipher what’s considered an abortion, when conception starts, and ultimately, what kind of care and services are safe to offer.
As states continue to pass laws prohibiting abortion, the real threat is the threat of the unknown because not every abortion law specifies that IVF and fertility won’t be affected moving forward, while others do. For example, South Carolina and Alabama specifically exempt IVF procedures from their abortion bans, Alabama citing that life begins when “a fertilized egg attaches to a uterine wall.” Meanwhile, other states are attempting to pass legislation that would grant embryos “personhood rights,” and in some cases, constitutional rights. This lack of clarity leaves IVF, its patients, and practicing physicians in limbo, begging the question of why IVF wasn’t more considered when writing these laws. With so many unanswered questions still looming, certainty is greatly needed to ensure the well-being of all Americans.

The Impacts on Patients
For those currently or planning on undergoing IVF, the possible adverse outcomes cannot be ignored, especially when it comes to a patient’s health if the implanted embryos do not result in a live birth.
“The important piece to understand here is that pregnancies can go awry and need to be resolved via abortion care,” explains Berson. “For example, ectopic pregnancies, where the baby is growing in the fallopian tubes, can result in death to the parent if the pregnancy isn’t terminated. Also, missed miscarriages—when the baby stops growing, but your body doesn’t realize–need to be resolved via abortion care or a [dilation and curettage] (D&C).
Berson, who founded Conceive after her harrowing journey through IVF, has her finger on the pulse of what patients are dealing with today, citing stories of pregnancy loss where patients couldn’t receive the care they needed because of abortion bans, and those suffering miscarriages only to be turned away from emergency rooms. She also reflects on a story where someone was denied access to their prescribed fertility medication over concern it could be used to end a pregnancy.
But miscarriage—particularly missed miscarriage, when a fetus has died or has not developed—has created a difficult gray area for patients and physicians to navigate. This is due to “when patients want and need a D&C, but it gets technically classified as an abortion, and they’re turned away from getting the care they need. At worst, there have been stories of people walking around with non-viable pregnancies for weeks, and at even worse, deadly ectopic pregnancies,” explains Berson.
In addition to pregnancy loss, a multiple pregnancy, which occurs in roughly 21.5% of pregnancies involving ART across all age groups, is also of concern, says Eshed. “Multiple pregnancy as a result of IVF may increase risk [of complications], prompting a medical decision to perform selective reduction, in which a fetus is terminated to allow for the other fetus or fetuses to have a healthy full-term gestation while lowering the risk of complications to the parent. In order to make informed decisions about their own health and well-being, people must have access to a variety of reproductive health services, including abortion care, and physicians must have the authority to act in the best interest of the patient.”
Whether someone is facing a multiple pregnancy or is considering the possibility of one as the result of IVF, abortion bans are making family planning for the future difficult, if not grim. “In this new world, there’s a possibility that in states where abortion is illegal, [patients] could be forced to carry that embryo(s) to term or pay for the storage of embryos in perpetuity. It then follows that those who discard embryos could be convicted of manslaughter for doing so,” warns Berson.
For IVF patients needing a D&C, selective reduction, or any other related procedure, they may encounter the obstacle of decreased access to physicians and facilities due to high demand and overwhelmed clinics, or clinics no longer offering reproductive services. This is due in part to patients being forced to travel to states with fewer or no abortion restrictions. What’s more, the addition of travel time and expenses associated with seeking care out of state may also deter in-need patients from receiving the help they require.
But that’s not the only associated cost. For patients living in states with bans and trigger laws, the potential legal consequences for seeking such procedures may require the presence of an attorney for guidance in understanding and interpreting the vaguely written laws on reproductive health care. With average lawyer fees ranging from $100 to $500 per hour, this additional protective measure could have crippling financial effects on families. Resources like the National Women’s Law Center have set up abortion access legal defense funds to aid in helping pay for legal fees associated with abortion care.
Another important aspect to consider is the emotional impact that comes from shouldering the burden of the fear of realities and future possibilities concerning IVF, such as weighing the consequences of a multiple pregnancy or being forced to travel across state lines to receive care.
“The mental and physical toll for those trying to get pregnant is already vast without these daunting prospects. At best, these new laws could limit the access and ability to get pregnant for people in those states; at worst it introduces the unnecessary and traumatic process of carrying non-viable embryos to term. It may come down to suggesting members move their embryos to states where they have more rights, but it’s not always easy as clinics have different methods for thawing and freezing. This is all murky right now, and we will be watching closely and updating our community as it unfolds,” says Berson.
The Impacts on Physicians
As previously mentioned, the ambiguous language used in some of these repeal laws creates confusion surrounding understanding what’s legal and what’s not; and in a physician’s case, what they can and cannot provide a patient, no matter how dire the circumstance, creating a moral burden of having to turn some patients away.
“As physicians and clinics struggle to understand the laws that are specific to their state of practice and the legalities they must take into account while upholding their ethical obligations to first do no harm, the Roe v. Wade decision can have a significant impact on medical practice and patient care, not just in abortion clinics but also in emergency rooms, oncology care, and labor and delivery units,” explains Eshed. “Doctors in emergency rooms may be hesitant to provide necessary medical treatment to pregnant people if they believe it could potentially result in a miscarriage or termination of the pregnancy out of fear of legal repercussions. Similarly, obstetricians and gynecologists who work in labor and delivery units may be hesitant to provide necessary medical interventions, such as induction of labor or cesarean section (C-section), if they believe it could result in the termination of a pregnancy.”
For fertility specialists, specifically, the argument of the embryo—whether it’s a person or property—is still the center of the conversation in determining what’s considered criminal. Berson mentions the possibility of doctors facing legal ramifications for simply educating patients on their reproductive options and advising them accordingly—which could be viewed as aiding and abetting a ‘crime.’ But there are other questions surrounding genetically testing and/or discarding embryos, and how criminal charges against these procedures would impact physician care and patient outcome.
Dr. Sable notes that anecdotally, there’s not much to go off to determine what kind of impact the overturning of Roe is having on clinics and physicians. “Are patients choosing to travel to clinics in non-affected states? Are patients transporting embryos out of state? Little to no data on these questions [is currently available].”
Still, it’s worth reiterating that the unknown is exactly what makes this situation so unnerving. Clearer laws are needed first and foremost, but until then, patients and their doctors are left to decipher information and try to make the best decisions possible.
“Ultimately, laws based on political and ideological reasons rather than medical necessity cause a burdensome conflict for health care professionals and their responsibility to put the best interest of the patient first,” says Eshed.
The Impacts on Maternal Health
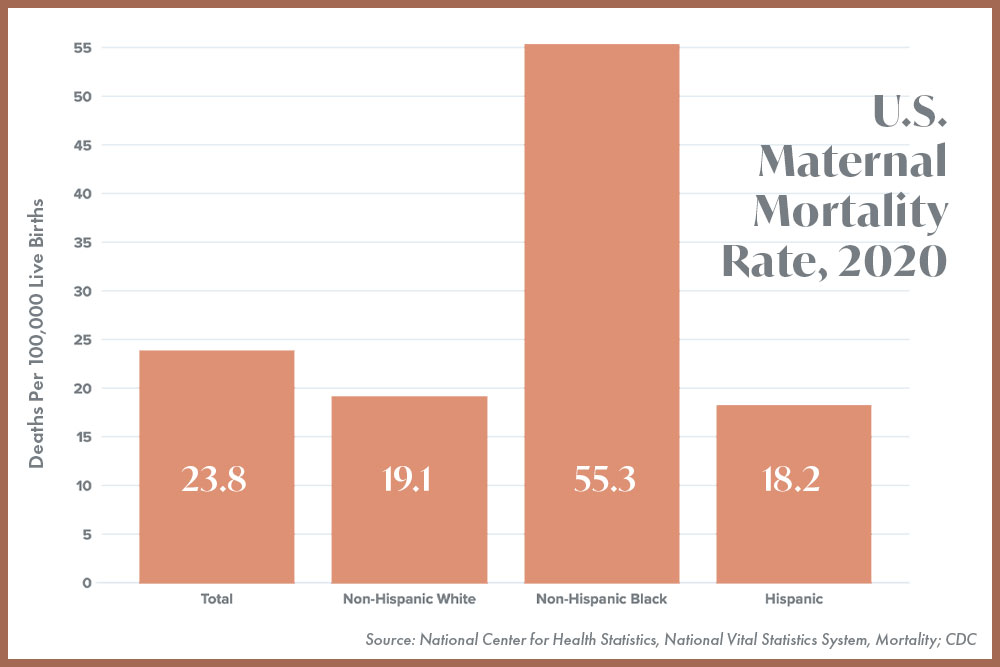
Indisputably, restrictions on reproductive care—including fertility care—result in consequences for maternal health. The U.S. already has one of the highest maternal mortality rates among high-income countries, but researchers have found that if access to abortion is restricted throughout the country, the overall number of maternal deaths would increase by approximately 24%. Even more alarming, they found that maternal death for Black women would rise by 39%.
According to Berson, the current realities for Black women undergoing IVF are also disheartening. “Black women have a 33% reduced rate of pregnancy through IVF and twice the rate of miscarriage from IVF. We’re also seeing stories like this harrowing NPR piece highlighting the dangers of pregnancy post-Roe for Black women in America, who already suffer from disproportionately higher rates of maternal mortality than their white counterparts. Meanwhile, this analysis from The Commonwealth Fund found a correlation between higher abortion restrictions and maternal and infant mortality rates. Maternal deaths in states that restricted abortion were 62% higher and many are maternity care ‘deserts.’ This puts women of color at disproportionately higher risk [overall].”
Additionally, a post-Roe world may mean fewer doctors in states with abortion bans, as out-of-state hiring has become tougher, according to recruiters. Retaining specialists in obstetrics and gynecology is another part of the equation, with more doctors reluctant to work in states where laws could limit their practice.
According to the Association of American Medical Colleges (AAMC), the U.S. was already facing a physician shortage before 2020, but “the COVID-19 pandemic highlighted many of the deepest disparities in health and access to health care services and exposed vulnerabilities in the health care system,” said AAMC President and CEO David J. Skorton, MD. “The pandemic also has underscored the vital role that physicians and other health care providers play in our nation’s health care infrastructure and the need to ensure we have enough physicians to meet America’s needs.”
Furthermore, potentially criminalizing and jailing doctors for performing certain procedures will result in fewer available doctors to provide care to everyone.
Future Considerations
If you are a current or potential IVF patient living in a state with abortion bans or restrictions, Berson, Eshed, and Dr. Sable all agree that having a prompt conversation with your provider is essential to understanding the laws and regulations that may impact your treatment. Additionally, Eshed adds, “It is also important to understand the policies and protocols of your provider and discuss how they are in compliance with the state laws and regulations, so you can decide if you are comfortable with the laws, policies, and protocols of the clinic, and that you are making informed decisions about your fertility treatment.”
In addition to preliminary questions you’d ask your doctor about the IVF process, Eshed also offers the following to help guide your conversation with your provider:
- How do you select an embryo for transfer?
- Do you use time-lapse incubation in your lab?
- What options or technologies, such as AI decision support tools, are available to promote increased success rates? Do you use them in your practice?
- What are the laws and regulations regarding IVF and abortion in this state?
- What happens to unused embryos? Are there any regulations or laws that govern the storage, donation, or disposal of embryos?
- Are there any restrictions on access to birth control methods after IVF treatment?
- Are there any legal requirements for the patients that they must have written consent in case of unused embryos or egg donation?
- Do you provide access to a legal specialist to assist in making an informed decision based on the current state law?
- What is the legal status of an embryo in this state?
- What is the process for freezing embryos and how long can they be stored?
- Are there any options for genetic testing of the embryos or eggs before transfer?
- Are there any restrictions on the number of embryos to be transferred?
- Are there resources to support patients during the IVF process, both emotionally and physically?
Another question to consider is whether you can benefit from telemedicine when weighing your options for care, especially if living in a state with bans in place.
Sophia Yen, MD, MPH, co-founder and CEO of Pandia Health, a birth control delivery and telehealth service provider, says it’s important to know that if you are in a state where abortion is illegal, then doctors from another state cannot legally help you. “However, there are trustworthy companies, specifically Access Aid, working from the Netherlands and India, that can provide medication abortion up to 10-12 weeks. You can also check out Plan C Pills and Mayday Health,” she says.
Actions We Can Take
We know seasons of uncertainty can feel paralyzing, and it’s OK to recognize that these are unprecedented times.
“The fertility world has been left wondering what the ripple effects will be pre-pregnancy. While we are still learning, and laws are still evolving, there is a potential to derail the momentum gained in the sector over the last couple of decades,” says Berson. However, there are steps we all can take to help continue progress.
Start by contacting your representative and demanding changes to the laws in your state (if applicable). Next, Berson says to support pro-choice political candidates, distribute abortion pill materials, check out Planned Parenthood’s Guide to Action, and organize demonstrations. She also shares Conceive’s Reproductive Resource Guide which seeks to “inform and empower individuals in their post-Roe v. Wade fertility decisions and engage companies in dialogue that leads to expanded fertility benefits and support for their employees.”
Other action items include:
- Talking about abortions as essential health care: By changing the conversation surrounding abortions, we can reframe how this form of care is perceived and remove political and emotional narratives.
- Donate to organizations that are fighting for reproductive health care: Berson lists Planned Parenthood, Doctors For Fertility, Resolve, the American Society for Reproductive Medicine (ASRM), and the National Network of Abortion Funds as great options.
- Find a like-minded community: Conceive is a great resource for helping you find a doctor you can trust, getting connected with others facing similar challenges, and staying up to date on changes in the IVF space.
There is no clear-cut answer here, as there is no perfect protection for physicians and anyone seeking reproductive health care. But we must be better informed to make more thoughtful decisions moving forward—because decisions about essential health care impact everyone.








