An Unplanned C-Section for Mom with Diabetes

One mother’s story of meeting her big baby boy, Eli.
By Kendyl Gray
First, I should start by mentioning that I am a Type 1 diabetic, so my first pregnancy was high risk. Before even getting pregnant I made sure my body was ready. I lowered my A1C—a measurement of how well my diabetes is managed—by getting on an insulin pump and a continuous glucose monitor, so basically, I became part robot. I wanted the healthiest pregnancy possible because there are risks when it comes to Type 1 diabetes, including heart defects, neonatal intensive care unit (NICU) stays, low blood sugar, and the scariest: stillbirth. But, this isn’t Steel Magnolia times; diabetics have healthy babies all the time because now there are better ways to manage the disease.
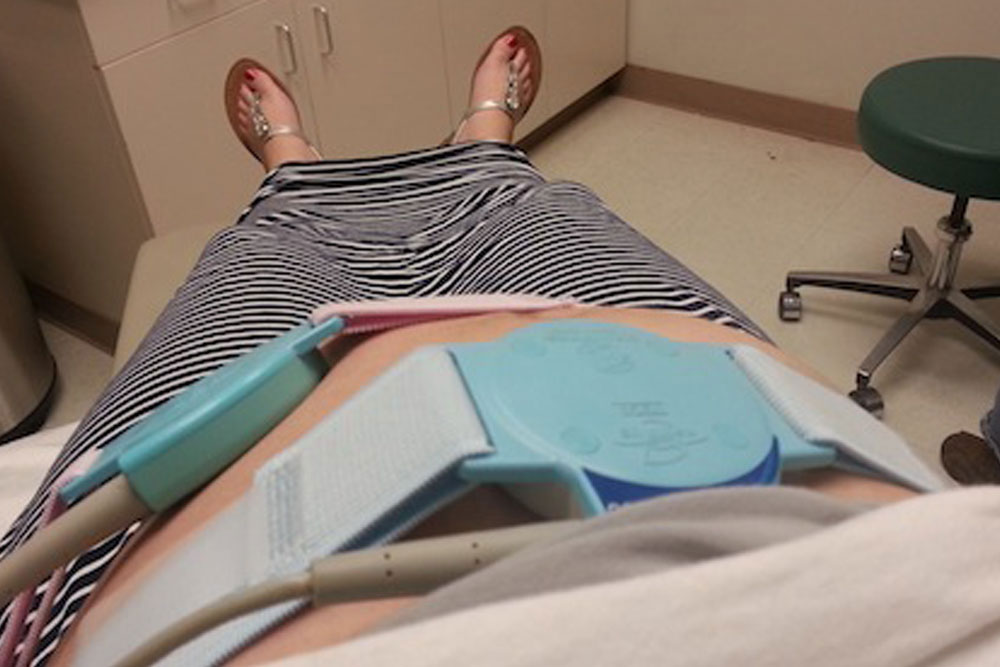
Because of my diabetes, there was a lot of monitoring. In the beginning, when most moms have one prenatal appointment, I had two. Towards the end, I was basically living at my OB-GYN’s office. Beginning around 28 weeks, I started weekly non-stress tests—or NSTs. This is when they put a monitor on your belly that measures baby’s heart rate and your contractions, and you get a little button to push every time baby moves. Most of the time, I just sat there for an hour listing to Eli’s heart rate and knitting. It was actually very relaxing. At around 31 weeks they noticed I was contracting every 15 minutes, except I didn’t realize I was having contractions. So they checked me and I was 1 centimeter dilated. I then thought, well, it won’t be long now.
False (Labor) Alarms
I had my baby shower around 34 weeks and got most of what we needed. At 35 weeks I went in for the NST, and my baby, Eli’s, heart rate was sitting at baseline at around 200 bpm. Every 10 minutes the machine kept beeping and alerting the nurses. They decided to send me to labor and delivery (L&D) for longer monitoring. I was also having contractions every five minutes. They checked me and I was 3 centimeters dilated. I went to L&D and waited four hours. Thankfully Eli settled down. Contractions continued but they were not painful. I was not changing so I was sent home and told to relax.
At 36 weeks I was sent to L&D again after the NST showed I was having contractions every two minutes. I was 4 centimeters dilated and 80 percent effaced. I was given tons of water and relaxed for four hours while I was held in pregnant-lady jail. They checked me several times, and I thankfully did not change. It was determined I had an irritable uterus and would probably contract till he was born. I then went home, packed my hospital bag, and installed his car seat. After I did this the contractions almost stopped completely! So, apparently, he was determined to come when we were not prepared at all.
I started trying to bring on labor—and I tried everything! I ate so much pineapple, was drinking red raspberry leaf tea, and taking evening primrose oil. Nothing was working. I so wanted my water to break sporadically. I just dreamed of being at a store (mainly so I wouldn’t have to clean it up) and then rushing to the hospital. But even with the irritable uterus, little man seemed to be quite comfy in there.
From 36 weeks on, I started doing twice-weekly NSTs. On November 8, I was 38 weeks and went in for my second NST that week. I had noticed that little man had not been as active the past couple of days but didn’t think much of it. My husband went with me because they had been sending me to the hospital so often. He packed the car with our bags and we headed off to the doctor. We had our ultrasound to measure Eli and make sure he was still head down. He was measuring 8.5 pounds and had been head down the entire pregnancy. They said the placenta looked OK, not amazing but OK. I then went to another room for the NST. The jelly they put on my enormous belly was warm. They found his heart rate immediately and his baseline was 160. He was normally on the high side of normal. They then put the contraction monitor on and gave me the button to push when he moved. Stephen and I sat there waiting.
It’s Go-Time
Honestly, I was hoping this wasn’t the day, but I knew deep down it was. It was the same birthday as my mother-in-law and I wanted Eli to have his own birthday. The doctor came in and looked at the sheet. He asked me about movement, and I told him Eli had not moved much in the past couple of days. He then said that there had not been the normal increases in heart rate, so they wanted to “buzz the baby.” I said OK but wondered what that meant. A nurse then came in and held a little thing to the bottom of my belly and literally buzzed Eli. Eli did not move, and his heart rate did not change. After another 20 minutes of no change, the doctor came back and said to go to L&D—we were having the baby soon.
Stephen had left his phone charger at home, so I asked how serious it was. I also explained that today was not a good day. He said it was not an emergency, but diabetics’ placentas tend to degrade faster—so it was just time. But we could go home to pick up what we needed and then head to the hospital.
I called my parents because they were two-and-a-half hours away and told them to head our way. We went home, grabbed my husband‘s charger, and I did the dishes. I was so not ready. We drove to the hospital, got to our room, and settled in. I was examined and was almost 5 centimeters dilated and 90 percent effaced. I was given another ultrasound and told Eli was 9 pounds, 1 ounce. I thought, there is no way he is that big because our ultrasound earlier said he was only 8.5 pounds.
We then called Stephen’s parents and let them know what was going on. I told Stephen that I really did not want a whole lot of people in the waiting room because I knew there was a very large possibility that Eli would have to go to the NICU for low blood sugar, and I wanted what time I had before they took him to do skin-to-skin and try breastfeeding. I told him only his parents and my cousin were allowed.
They started the Pitocin around 3 in the afternoon. The contractions started coming hard, and my Dexcom (continuous glucose monitor) started beeping at me. I looked at it and saw 50 with double arrows down. That meant my blood sugar was low and dropping fast. I called the nurse and told her, so she gave me some dextrose. With the Dexcom still yelling at me, I checked again 15 minutes later, still low. I called the nurse again, and they doubled the dextrose. Again 15 minutes later, STILL LOW! So they gave me juice, and I turned my insulin pump completely off. I then started throwing up. Just so you know, I threw up twice a day the entire pregnancy, so it was only fitting that I thought I was going to throw Eli up.
At this point, Eli’s heart rate was dropping with contractions, I was yelling and shaking the bed rails—and vomiting. This was not what I thought it would be like, but it was too late to turn back. They finally gave me Phenergan, and my blood sugar held stable at 80. The nurses thought it should be higher, but there really wasn’t anything we could do. I was told I had to lie on my side and I was given an oxygen mask. I asked for an epidural because I couldn’t move. Thankfully they also gave me some other pain meds to hold me over until the anesthesiologist came. He gave me the epidural and I felt nothing, not even the needle going in. He really was amazing. I was checked again after and was around 8 centimeters. I just kept thinking, this has to slow down—he can’t be born today!
Eli’s heart rate kept dropping, so they decided to use internal monitors and break my water while also turning off the Pitocin for 30 minutes. I was told that they would only turn off the Pitocin three times before they would take him by C-section. Well, I continued to progress without the Pitocin. I took a short nap since I still had the Phenergan coursing through my veins.
During this time my parents and cousin left to get something to eat. My father-in-law and step-mother-in-law came by, said hi, gave their support, and then waited in the waiting room, thankfully. I really did not want an audience, and they respected my wishes of only wanting Stephen, my mom, and my cousin in the room. I am not very nice when I am uncomfortable. My parents and cousin came back, and thankfully my dad took my mother-in-law with him to the waiting room. I was checked again and was 9 centimeters at 11 p.m. OK, I thought, one more hour; I can hold him in for ONE MORE HOUR!
The Big Reveal
The nurses came in and turned his bed warmer on. They started getting everything ready for me to start pushing. The doctor checked me again, and I was 10 centimeters—but Eli was still too high, so they put me in different positions to try and make him drop, like the Texas Roll.
Midnight came and went. (Yes! He would have his own birthday!) They tried many different positions, and the epidural was wearing off.

At 5:30 a.m. the doctor came in and told me to push. She then said, “Honey, he isn’t coming down. I think you need a C-section.” At that point, I just wanted him out, be it a cesarean or a vaginal delivery. I was totally exhausted.
At 6 a.m., the anesthesiologist came in and gave me something stronger than the epidural. It was amazing. I felt nothing.
Stephen changed into scrubs, and we were wheeled to the operating room (OR). Since I was giving birth for the first time in a teaching hospital, everyone and their dog were in the OR. When a baby is born the entire pediatric team is called to the birth, so we had a large crowd watching.
I was so tired. As they were prepping me for my C-section birth, I rested my eyes. Stephen came in, and I was told I might feel pressure. I don’t know if the epidural was just so good or if I was so tired, but I felt nothing. No tugging, no pulling, no pressure. Eli was pulled out of me, and I heard from every nurse and every doctor, “Wow, what a big boy!” The anesthesiologist whispered to me, “Honey, he was never going to fit.” And then I heard the most wonderful sound in the world: his cry.
They held him up, and he had a head full of dark hair and the chubbiest cheeks I had ever seen! Stephen held him up to my face, so I could kiss those sweet, chubby cheeks. A nurse snapped a picture for us. We both looked so exhausted—but so in awe of our adorable little boy. They cleaned him up and took him to be measured. I was stitched and stapled and then wheeled to recovery. He was 9 pounds and 1 ounce of perfection.
Unfortunately, he had low blood sugar, and I only had 30 minutes with him before they took him to the NICU. I didn’t get to have a chance to bond skin-to-skin or to try to breastfeed him before I was bombarded with visitors. However, I was the lucky one that morning because I was a new mom, and my baby boy was alive and healthy.
Eli was taken to the NICU and given an umbilical IV. They also discovered that he had air pockets in both lungs. After 12 hours, I was finally able to go downstairs and hold him. The NICU nurses were wonderful. They loved him because he was big enough to hold. He wasn’t as fragile—just could not control his blood sugar as well. After a day his blood sugar stabilized, but we had to stay five days for his lungs and to wean him off of IV fluids. Being in the NICU made us even more grateful for our healthy baby boy.
Today, Eli is a wild 1-year-old who is smart, stubborn, and so sweet. He chases the dogs all day, loves to give hugs and kisses, and jabbers up a storm. As he lies sleeping next to me with the messiest blonde hair, I can say he has changed me for the better. He has taught me to just roll with the unexpected and be thankful for every day. I am especially thankful for my birth story because it made me his mother.
Send us your birth story! Whether you had a home birth, hospital birth, 37-hour labor or emergency C-section, we’d love to read the tale of your little one’s grand entrance. Write up your birth story (click here for tips on getting started) and email it, along with a few photos, to birthstory@pnmag.com, and we’ll share it on our site!*
*By submitting your birth story to Pregnancy & Newborn, you’re granting our editorial team permission to share your story details and personal images, and to edit the story as needed.







